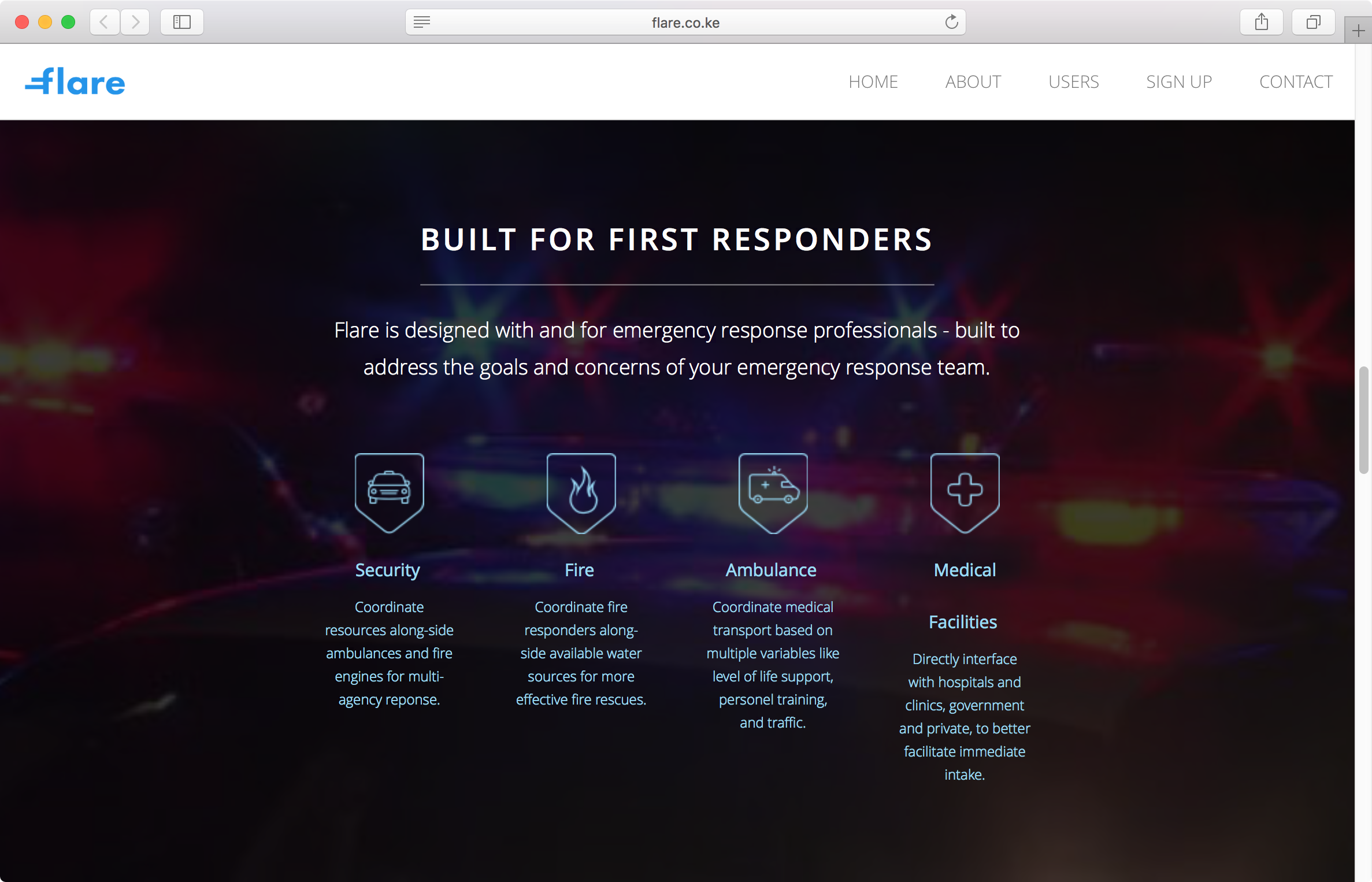
Emergency Response
Platforms that link people to the full range of public and private emergency response services through one interface, matching people in urgent need with the closest and best equipped vehicles and mapping their routes to-and-from the incident.
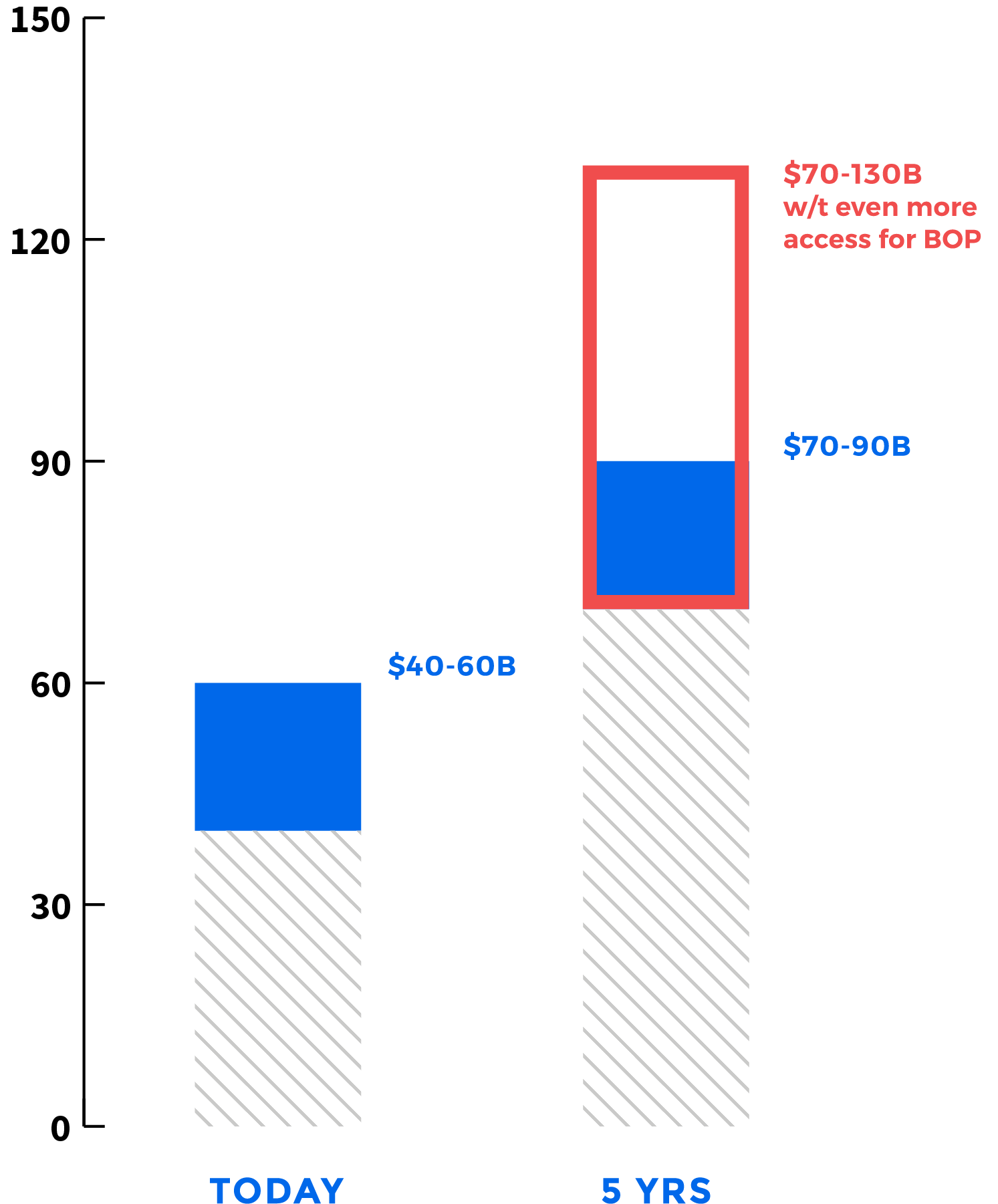
Potential Market Size (by 2022):
70-90 Billion USD; 2-3 Billion Users